In the article, we consider what a condition such as retinal stratification is.
The retina is responsible for the interaction between the brain and the eyes. Its main role is the conversion of light signals into nerve impulses. In case of impaired functioning or detachment (when the choroid and retina are separated), vision deteriorates and the quality of human life suffers.
Causes
Retinal stratification can be either primary or secondary. The main cause of the primary type is retinal rupture and fluid accumulation in the areas of its exfoliation. The source of secondary exfoliation is various neoplasms. So, predisposing factors are:
- stress situations;
- circulatory disturbance;
- viral diseases;
- human ophthalmic interventions;
- retinal dystrophy;
- too much physical activity;
- injuries of the organs of vision;
- high degree of myopia;
- diabetes;
- pregnancy.
The reasons for the separation of the retina should be determined by the doctor.
Symptoms
If a person knows the first symptoms of retinal stratification, he will be able to go to the doctor in time and prevent serious complications. These signs are:
- the appearance of a shadow or veil in one of the fields of vision, when moving the head, it can fluctuate;
- the appearance of a large number of black dots in the field of view, indicating areas of blood flow in the vitreous body;
- a feeling of sharp bright “flashes”, “sparks”, “lightning” (such “visions” are mainly observed in the eye area, which is located closer to the temple).
The signs of retinal stratification listed above will be accompanied by visual impairment. The patient may notice the curvature of the lines and shapes of objects. If the retinal detachment is fresh, a syndrome of improvement in the quality of vision in the morning may be noted. This is because the liquid that accumulates in the areas of exfoliation dissolves slightly during the night. Most patients think that such symptoms are a sign of fatigue, and therefore a visit to the ophthalmologist is postponed, and the process begins to progress at a rapid pace.
If the pathological process occurs in the upper parts of the eye, then the symptoms of retinal stratification spread much faster than in the lower ones. This is explained by the fact that, according to physical laws, the accumulated liquid begins to sink down, causing retinal detachment in the departments located below. In these parts of the organs of vision, retinal tears are dangerous because they can occur for a long time with almost no symptoms, revealing themselves only after spreading to the central (macular) region of the eye. The type of retinal detachment affects the severity of symptoms. It gets the most expression with regmatogenous detachment, while with an exudative or traction variety, the manifestations are more scarce, which slowly develop and are diagnosed only after damage to the ocular macula.
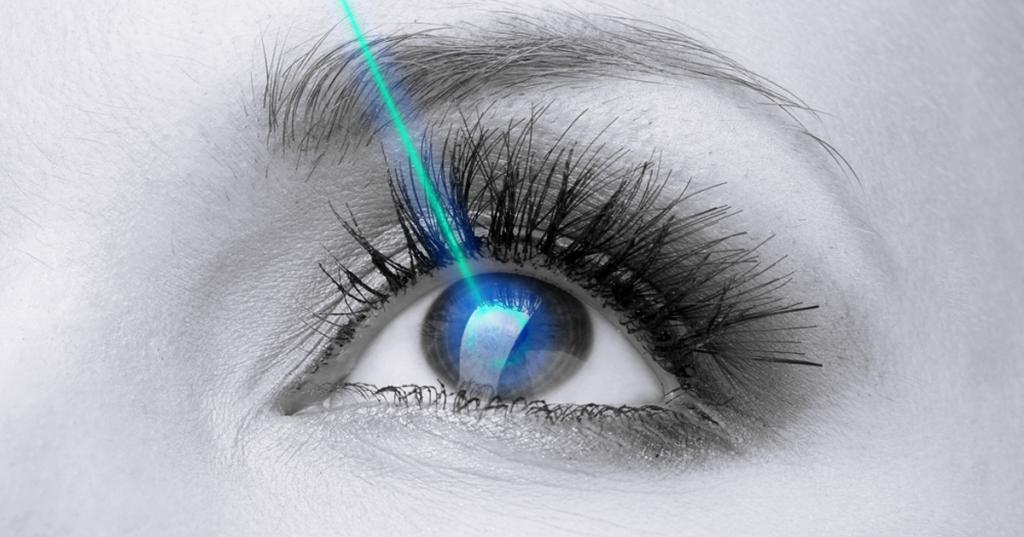
Retinal stratification in the photo is difficult to convey.
Diagnostics
If there is the slightest suspicion of stratification of the retina, a thorough eye examination is performed. Diagnostic methods are divided into three types: special, standard, laboratory. Standard methods include:
- perimetry - analysis of the field of view in order to establish its boundaries and diagnose defects (cattle);
- tonometry - determination of pressure inside the eye;
- Visometry - establishing visual acuity through special tables;
- ophthalmoscopy - analysis of the fundus using an ophthalmoscope and fundus lens to assess the condition of the optic disc, retina and vessels of the fundus;
- biomicroscopy - a thorough examination of the eye structures, which is performed using a slit lamp;
- analysis of entopic phenomena - makes it possible to assess retinal function retention.
Specific studies include:
- Ultrasound in B-mode - allows you to view in two dimensions the eyeball and visualize the contents of the latter and the orbit;
- EFI (electrophysiological methods) - these include electroretinography, electrooculography and electroencephalography, which records the sensitivity of the optic nerve and the associated potentials of the visual region of the brain cortex.
Laboratory research methods may include:
- blood tests: for hepatitis C and B, HIV, syphilis, general, biochemistry;
- urinalysis - for sugar and general.
Of particular importance in the diagnosis of retinal detachment is ophthalmoscopy. With the help of such a study, it is possible to establish the extent of exfoliation, the location of the areas of breaks and retinal degeneration, shape. Retinal detachment ophthalmoscopically manifests itself in the disappearance of the normal red reflex at the bottom of the eye in one of its zones. In the area of exfoliation, it acquires a grayish-white color. With long-standing detachment, coarse folds and star scars appear on the retina. The retina becomes detached and rigid during detachment. The areas of discontinuity appear in various shapes and red. The use of all methods of examining the organs of vision in the aggregate makes it possible to obtain the most informative picture, allowing you to draw up the most effective and adequate treatment plan.
Treatment and recovery
The only effective way to retinal stratification is surgery. Carrying it out at the very early stages of this pathological process allows you to get the best results, increases the possibility of restoring lost vision. The main goal of treatment is to block the gaps existing in patients, reduce the volume of the eyeball and restore interaction between the exfoliated areas.
Surgical interventions to eliminate retinal detachment are divided into:
- laser;
- endovitreal;
- extrascleral.
The tactics of surgical therapy are selected purely individually, depending on the degree and causes of retinal detachment.
Effective eye drops for retinal dissection:
They have the same effect. However, "Emoksipin" gives an unpleasant burning sensation, causing discomfort. Therefore, if "Emoksipin" did not suit you, then it is possible to replace it with "Tauron". Of course, before using these drugs, you should consult an ophthalmologist, and in the process of their application, monitor the change in condition.
Extrascleral treatments
The operation with extrasclerral methods of surgical therapy is performed on the surface of the sclera. These techniques include filling and ballooning.
What does the first method mean? This procedure is performed on the surface of the sclera, its main purpose is based on the convergence of the surface of the pigment epithelium and the exfoliated area of the retina. Prior to surgery, the exact exfoliation zone is determined. The required size of the seal is made of soft silicone sponge. The surgeon cuts the conjunctiva and imposes the prepared element on the required area of the sclera. Depending on the type of retinal detachment, filling can be performed according to a sectoral, circular or radial technique. If necessary, the accumulated liquid can be removed. Some clinical cases require the introduction of special gas or air into the cavity of the eye. After the intervention is completed, the surgeon will stitch the conjunctival incision. This operation may be complicated in some cases. So, in the early period after the intervention, the following can be noted: infection of the surface of the wound, impaired functioning of the oculomotor muscles, detachment of the lining of the vessels and lowering of the upper eyelid, increased pressure inside the eye. In the late period after surgery, the following are possible: exposure of the implant, development of cataracts, the formation of membranes, degenerative foci and microcysts in the macula area, as well as a change in ocular refraction towards myopia. If the extrascleral filling procedure is performed unprofessionally, then there may be no tight fit of the stratified area and repeated retinal detachment.
After extrascleral filling intervention, vision is restored within two to three months (a longer period in old age). In most cases, it will be incomplete, which depends on the age of detachment and the degree of pathology of the central part of the retina. The price of extrascleral filling is determined by the prestige of the medical institution and the volume of procedures performed.
What is extrascleral ballooning? A balloon with a special catheter is inserted over the eye during the procedure. Using a balloon, pressure is applied to the sclera, the inner shell is fixed with a laser. The balloon is removed five to seven days after laser coagulation. Extrascleral ballooning in some cases can be complicated by increased values of intraocular pressure, hemorrhages and cataracts.
Contraindications of such an operation are:
- extensive tear line breaks and tears;
- fixed folds that occupy more than ¾ of the fundus;
- rupture is complicated by the outpouring of blood into the vitreous body.
Such an intervention is less traumatic, carried out for 30-50 minutes. Its effectiveness is determined by the timely appeal to the doctor and can give positive results in 98% of cases. The cost of the procedure depends on the medical institution where it is performed and the severity of the state of the retina.
What else is the treatment for retinal stratification?
Endovitreal treatments
The endovitreal operation is performed inside the eyeball. This operation is called vitrectomy. By it is meant the partial or complete removal of the vitreous. Thanks to this, the surgeon gets access to the posterior wall of the eye cavity. Subsequently, the pulled vitreous is replaced with a special material that must have the desired degree of viscosity and high transparency, be hypoallergenic, long-term and non-toxic. For this, in most cases they use special balanced salt solutions, bubbles with gas or oil, artificial polymers.
Vitrectomy has the following contraindications:
- gross violations of the optic nerve or retina;
- pronounced corneal opacification.
During vitrectomy, the surgeon removes the necessary areas of the vitreous body through very thin punctures. Then, laser coagulation of the zones of the retina is performed, detachment is compacted, the integrity of the retina is restored. A substitute for the vitreous body is inserted into the formed cavity, which keeps the retina in a normal physiological state. Possible complications of vitrectomy: lens defects, bleeding, detachment or tearing of the retina. In the period after the operation, there may be repeated hemorrhages, the development of inflammation, increased pressure inside the eye, changes in the cornea, as well as repeated retinal dissection. The operation can last from one and a half to two to three hours. This type of intervention has proven itself as an effective way to preserve and restore vision. The cost of this surgical technique is determined by the following circumstances: eye condition, authority of the medical institution and the nature of the intervention.

Laser treatment
Therapy of retinal stratification with a laser can be carried out only at its initial stages. This procedure is called peripheral restrictive laser coagulation. It is aimed at preventing retinal separation. Its essence is based on the action of the laser beam on the thinned disturbed areas of the retina. Laser radiation “solders” them, forming soldering of the retina and tissues located below. Restrictive peripheral coagulation ultimately leads to an increase in blood flow velocity, normalizes nutrition and blood supply to pathological areas of the inner ocular membrane, and blocks the flow of fluid under the retina. Two weeks after surgery, you can perform vision correction with a laser.
The use of a laser for retinal stratification has the following contraindications:
- gross changes in the fundus of the eye;
- the presence of obvious epiretinal gliosis (a film forms on the retina);
- gross rubeose (pathological vascular growth) of the retina;
- insufficient transparency of optical media.
Intervention can be carried out in a stationary and outpatient setting for one session. It lasts from five to fifteen minutes. Patients tolerate the treatment of retinal stratification by laser surgery easily, it is not complicated by anything. The cost of restrictive peripheral coagulation is determined by the area of the retina exposed to the laser, as well as the authority of the medical organization.
Folk remedies
Traditional medicine uses the following tools:
- blueberries (raw inside as an antioxidant);
- mistletoe (you need to make a decoction and drink it - it reduces pressure inside the eye);
- elderberry (for washing the eyes);
- eyebright (for compresses);
- fennel (for lotions);
- blackberry (ingested - antioxidant, contains vitamin C);
- hawthorn (used in the form of tincture, thanks to it oxygen nutrition and blood circulation of tissues are improved).
When retinal detachment is strictly prohibited replacement of surgical intervention with alternative medicine. They will not cope with the violation that has begun, but will only alleviate the symptoms and slow down the course of the disease.
Attempts to treat folk retinal stratification can significantly impair vision and lead to blindness. You should not waste time on such unreasonable therapeutic methods - at the first symptoms you need to urgently consult a specialist.
Consider the prevention of retinal stratification and its consequences.
Prevention and consequences
The main consequence of pathology becomes blindness. Surgery for this pathology should be carried out as early as possible, since only this method can help to avoid complete loss of vision and achieve its maximum recovery.
Unfortunately, few people know how serious the separation of the retina of the eye and its consequences.
The main preventive measure to prevent the ailment is a regular visit to an ophthalmologist by patients from risk groups (patients with diabetes mellitus, myopia, hypertension, who have suffered eye or head injuries, pregnant women, etc.). The frequency of such examinations is set individually (at least once a year), the doctor’s examination should include diagnosis of peripheral areas of the retina against the background of the dilated pupil. Such a group of patients should know the first symptoms of retinal detachment, so that when they occur, immediately seek medical help. If areas of dystrophy or rupture of the retina have been detected, patients may be given restrictive peripheral laser coagulation that can prevent the development of detachment. In order to prevent retinal stratification, patients may be advised to refuse to engage in heavy sports, somewhat limit the choice of professions and give special advice on the visual load on the eyes. If pregnant women have a risk of retinal detachment, then caesarean section is recommended for obstetric care. In order to prevent such a violation, patients from the risk group and other population groups need to observe the normal regime of visual and physical stress, not to lift weights, and to avoid injuries to the eyes and head.

Retinal Stratification Reviews
Patient reviews generally come down to the effectiveness of laser treatment, the discomfort during this procedure is much less than with other types of interventions, and the recovery period is much shorter. People talk about almost complete painlessness (although some claim that discomfort is present) and the success of treatment. Among the shortcomings, patients note a high cost of intervention, headache after and a burning sensation in the eyes. However, most consider this a trifle in comparison with possible blindness.
In principle, everyone definitely recommends the operation, since the detachment does not resolve by itself.